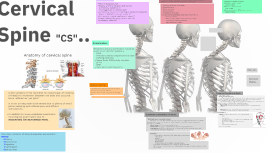
Cervical Spine...
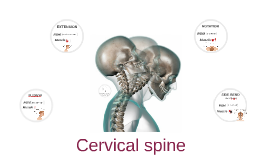
Transcript: Palpation: Observation: Patient History: Patient should be suitably undressed The therapist should conferm the patient's will to move Patient can be observed setted or standing Look for any abnormal Tenderness,Swelling,Edema or any abnormal Tempreture Facet joint Transverse process Mastoid process Temporomandibular joint Swollen lymph nodes Carotid pulse Sternum and clavical First 2 ribs Muscles such as SCM,trapezius and supraspinatus Patient Usual activity? Exactly where is the pain distributing? Is there any parasthesia? What aggravets or relieves pain? Is there any dizziness or fainting or headache(headache place is relatted to vary of causes )? Is there any muscle weakness or spasm? Is pain affected by coughing or sneezing? Is sleeping affected? 1-Position of head and neck 2-Shoulder level 3-Spine posture 4-Muscle bulks 5-Vasomotor changes any abnormal pathology that may affect th CS -Forward head -Tilted head (which indicates scoliosis) -Loss of Cervical curvature -Torticollis/Wry neck Cervical Spine "CS".. Examination: Anatomy of cervical spine Movement and any examination should be examine actively then passively: ROM (Flextion,Extention,Hyperextention,Sidebending,Rotation) Upper limbs ROM(mainly shoulder joint) MMT Dermatoms and Mayotoms Design at work... Almost there... Special Testing: * all needed special tests should be done in order to confirm or cancel medical diagnosis *be careful since this area is very sensitive and fragile area Common Disorders of Neck: * *Cervicogenic headache (CGH): is a chronic headache ( pain or discomfort in the head or face area ) that arises from the atlanto-occipital and upper cervical joints,It could be confused with a migraine, tension headache, or other primary headache syndromes. it can be challenging to diagnose because associated neck pain and cervical muscle tenderness occurs with many other headaches disorders. Main causes vary from arthritis to stauma of the neck Causes could be stressor pressure in neck structures ,over stretch and poor posture. Symptoms could be one side headache starting from occipital that spread to forehead some times causes neck pain and dizzeness Is the vertebra of the neck,that its responsepel of nodding of head,this movement between the atlas and occipital bone reffered as "yes joint". It is not an easy task to be tested due to plenty of small joints,radiating and reffered pain and diffrent articulations . In addition to musculoskeletal examinatio, neurological examination due to RADIATING OR REFERRED PAIN. Common Disorders of Neck: Treatment is conservative the main way is physicaltherapy US HEAT cervical collar joint mobilization(C1-C2 Mulligan Nutural ApophysealGlide) sofr tissue massages neck exercise (Deep Neck Flexor Exercises) ROM positioning and home advises NSADs could be taken *Whiplash Injury (nonmedical term) describes neck pain that causes injury to soft tissue (ligaments,tendons,muscles).It is caused by an abnormal motion or force applied to neck that causes movement beyond normal ROM Main Cause is RTA,some sports,fall injury Mechanism of injury is hyperextention followed by hyperflextion Symptoms starts from neck pain to CX fracture (dizziness ,shoulderpain,visual disturbances neck pain headaches Treatment Conservative treatment which dependes on semptoms: -neck collar -US or IF -gentel stretch -cryotherapy -ROM and some times gentel massage therapy If cervical spine fracture then surgery is recommended At the time of incident dont move the patient and keep his spine stable as much as possible The main contents of Musculoskeletal assessment : HOPES: History Observation Palpation Examination Special test