Rash Presentation
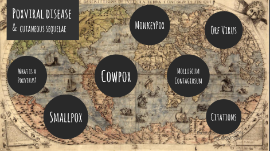
Transcript: "Doc, I've got this weird rash" Intro "Yeah that looks like some kind of rash" Dermatologist (noun) [dur-muh-tol-uh-jist] 1. From Greek, meaning "fake doctor" Rash: bad chief complaint, or the worst chief complaint? 1. Rash rules 2. Derm terms 3. Cases (in yo faces?) 4. Questions (rosh) 5. Questions (you) Overview Overview Caveats 1. It turns out that there is an entire specialty devoted to this 2. I cannot teach an entire specialty in 45 minutes, even this one 3. Most of this presentation will be talking about adult rashes 4. I'm going to assume you know what anaphylaxis looks like and what to do about it. Caveats Ross's Rash Rules (Recall that rules require some reservation) Ross's Rash Rules (Recall that rules require some reservation) 1. At least 95% of the rashes we see are not dangerous 2. Mucous membranes = bad 3. Rapidly progressive = bad 4. Systemic symptoms = bad 5. Skin sloughing off = bad 6. Palms/soles = bad 7. It's always lupus 8. It's never lupus 9. Come up with a rash script Questions to ask those with rashes Questions to ask those with rashes Meds (including recent abx/OTC meds) Travel Other new exposures (shampoo, detergent, etc) Hx of similar rashes Associated symptoms Exposure to others with similar rash Bugs/ticks Derm Terms (basic) Derm Terms (basic) Macule (patch) Papule (nodule) Vesicle (bulla) and pustules Plaque Don't call derm and call something a maculopapular rash. They will hate you. Defined as change in color, does not have texture. Macule <1 cm, patch >1 cm. Macule and Patch Macule and Patch Papule - raised, on surface of skin, usually <1 cm Nodule - raised, often under the skin, "better felt than seen", usually >1 cm Papule and Nodule Papule and Nodule Vesicle: raised, fluid filled structure <0.5 cm Bulla: raised, fluid filled structure >0.5 cm Pustule: raised, fluid filled structure filled with pus, usually <1 cm Vesicle, Bulla, Pustule Vesicle, Bulla, Pustule Well-circumscribed, raised, palpable lesion Plaque Plaque Find a way to organize "dangerous rashes" in your brain. Some suggestions: Drug reactions vs infectious vs autoimmune Appearance of rash (whole body erythema, bullae, urticaria, etc) Cases Cases Case 1 Case 1 32 y/o male presents to the ED. "I just got this weird rash". Being an astute clinician, you ask about new medications, and find out that he has bipolar disorder and was just started on a new medication. You see the following rash. What is your presumptive diagnosis, what do you think the offending agent was, and what do you want to do? Spectrum of disease - EM minor (who cares), EM major (care a little bit), SJS (ruh roh), TEN (if you send this home you messed up). Supportive care - fluids, electrolytes, burn center if SJS/TEN, stop offending med. Unclear if steroids/IVIG/cyclosporine might be useful. For EM major with mucosal involvement, most sources say give steroids. Causative agents include: phenytoin, carbamazepine, lamotrigine, phenobarb, sulfa drugs, allopurinol, NSAIDs Dx/Tx? Causative agents? Dx/Tx? Causative agents? Spectrum Spectrum Name this sign Name this sign You are hard at work in the pediatric ED having seen your 12th iteration of either "fever, cough" or "fever, ear pain" when suddenly "fever, rash" pops up on the board! You see an unhappy looking kiddo with the following rash. Case 2 Case 2 Staphylococcal scalded skin syndrome - and think about toxic shock syndrome. Caused by staph aureus (surprise!). Often prodrome of fever, skin pain, irritability though can be just sudden erythema. +Nikolsky sign. Treat with abx with MRSA coverage. If child looks well, is older than 1 year, takes PO and the case is mild, can try outpatient treatment. Otherwise admit for IV abx. Warn parents that most of skin will desquamate, but should grow back within 7-14 days. Dx/Tx? Dx/Tx? Case 3 (real!) Case 3 (real!) 48 y/o female with history of metastatic melanoma presents with fever, hypotension and the below rash after starting dasatinib 3 weeks prior. What is your workup and management? -WBC 12.6 with atypical lymphocytes -8% eosinophils -AST/ALT 157/138 -Cr 1.2 (baseline 0.7) Workup Reveals... Workup Reveals... DRESS syndrome (Drug Rash with Eosinophilia and Systemic Symptoms) -Typically 2-6 weeks after causative drug (allopurinol, seizure drugs, some cancer drugs) -Suspect if: morbilliform rash, hx of drug exposure in correct timeline, fever, facial edema, enlarged lymph nodes -As discussed, check labs including CBC, BMP, LFTs, consider checking trop (myocarditis). Pneumonitis is also possible. -Tx: STOP THE DRUG. If severe, can try steroids ~1-2 mg/kg of prednisone/day until improving, then taper. Dx/Tx? Dx/Tx? A 48 year old woman with mild rheumatoid arthritis presents with blisters "that have been there for a couple weeks, but got way worse the last 2 days. And they hurt really bad". On exam, you find the lesions below, near her lips. Case 4 Case 4 Dx/Tx? Dx/Tx? Highlights: -mucosa often first in pemphigus. -flaccid bullae, Nikolsky + -biopsy of intact