Pressure ulcer
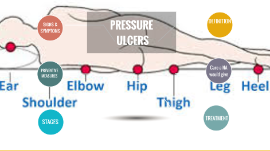
Transcript: stage4 stage 3 NHS reported that just under 25000 reproted to develop pressure ulcer from 2014 -205 20% of people in acute care & 30% of people in community at risk. pressure ulcer treatment is a costly process . The UK spends around 1.4 to 2.1 billion yearly. (Bennett, at al,. 2004). objective prevention pressure ulcer mostly occur as a result of inadequate care, following the principle of prevention help protecting people at risk from developing pressure ulcer Nonblanchable erythema of intact skin heralding lesion of skin ulceration. In individuals with darker skin, discoloration of the skin, warmth, oedema, induration or hardness may be indicators. kareema alabri References Thank you mobility problem poor nutrition underlying health condition being over 70 years old incontinence : urine/ bowel serious mental health condition Full thickness skin loss involving damage to or necrosis of subcutaneous tissue that may extend down to, but not through underlying fascia. The ulcer presents clinically as deep crater with or without undermining of adjacent tissue (Ellis, 2016) How it occurs The extra pressure disrupts the blood flow through the skin. Without the blood supply, the effected skin areas became starving of oxygen and nutritions.it began to breakdown leads to formation of ulcer which can be infected by bacteria. stage 2 content stages 1 areas of damaged skin and tissue that developed from sustained pressure usually laying in bed or sitting in wheelchairs. Range in severity from patches of discoloration skin to open wounds that expose the underlying muscle or bone . (Morison, 2001) (Ellis, 2016) Partial thickness skin loss involving epidermis, dermis, or both. The ulcer is superficial and presents clinically as an abrasion, blister, or shallow canter. (Ellis, 2016) sites (Keller, et al., 2002) At the end of this session the student will be able to define pressure ulcer. states the causes and how it occur. identify the sites and stages. list the measures to prevent it. (Ellis, 2016) Toward reducing the pressure ulcer incident throw implementing the prevention measurement. At risk Full thickness skin loss with extensive destruction, tissue necrosis, or damage to muscle, bone, or supporting structures (e.g, tendon, joint capsule). Undermining and sinus tracts also may be associated with Stage IV pressure ulcers. (NHS Choices information) Pressure ulcer Conclusion What is pressure ulcer How it happen At risk Sites and stages Braden scale Prevention Bennett, G., Dealey, C. and Posnett, J., 2004. The cost of pressure ulcers in the UK. Age and ageing, 33(3), pp.230-235. Bergstrom, N., 1994. Treatment of pressure ulcers (No. 95). DIANE Publishing. Cannon, B, & Cannon, J 2004, 'Management of pressure ulcers', American Journal Of Health-System Pharmacy, 61, 18, p. 1895, Academic Search Premier, EBSCOhost, viewed 24 November 2016. Lyder, C.H., 2003. Pressure ulcer prevention and management. Jama, 289(2), pp.223-226. Langer, G., Knerr, A., Kuss, O., Behrens, J. and Schlömer, G.J., 2003. Nutritional interventions for preventing and treating pressure ulcers. The Cochrane Library. Bergstrom, N., Braden, B.J., Laguzza, A. and HOLMAN, V., 1987. The Braden scale for predicting pressure sore risk. Nursing research, 36(4), pp.205-210. House, K.W. and Johnson, T.M., 2014. Prevention of Pressure Ulcers. In Pressure Ulcers in the Aging Population (pp. 27-45). Humana Press. Morison, M. J. (2001) The prevention and treatment of pressure ulcers. London: Mosby. Ellis, M 2016, 'Understanding the latest guidance on pressure ulcer prevention', Journal Of Community Nursing, 30, 4, pp. 29-36, CINAHL Complete, EBSCOhost, viewed 25 November 2016. https://i.ytimg.com/vi/9AvCUJgT2zI/hqdefault.jpg (accessed on 7/12/2016). http://www.nhs.uk/Conditions/Pressure-ulcers/Pages/Causes.aspx, (accessed on 7/12/2016). Keller, P.B., Wille, J., van Ramshorst, B. and van der Werken, C., 2002. Pressure ulcers in intensive care patients: a review of risks and prevention. Intensive care medicine, 28(10), pp.1379-1388. What is pressure ulcer? Aim